Main Complications of Cataract Surgery: Expert Guide by Neil Modi, FRCOphth

September 7, 2025
Comprehensive Insights into Cataract Surgery Risks, Symptoms, and Management
Learn about intraoperative and postoperative risks, symptoms, prevention, and expert management tips for optimal eye health outcomes.
Main Complications of Cataract Surgery: What Patients Need to Know
Cataract surgery, stands as one of the safest and most effective vision-restoring eye surgeries worldwide. While most patients experience excellent results, it’s important to be aware of potential cataract surgery complications. This article provides a detailed overview of the leading risks, how to recognise symptoms, and the best ways to manage and minimise these complications for lasting eye health.
What Is Cataract Surgery?
Cataract surgery involves removing the eye’s clouded natural lens and replacing it with a clear artificial intraocular lens (IOL). The lens capsule, a clear membrane in which the body of the lens sits, is left in situ. It is a 6 micrometre thick, transparent layer and it supports the new lens when it it placed in the eye.
Most procedures use phacoemulsification, a technique that utilises ultrasound energy for lens removal. Thanks to advanced technology, complication rates are low, but no procedure is risk-free. Understanding the main complications of cataract surgery is essential for patients considering this life-changing operation. The below diagram shows the steps of cataract surgery diagrammatically.
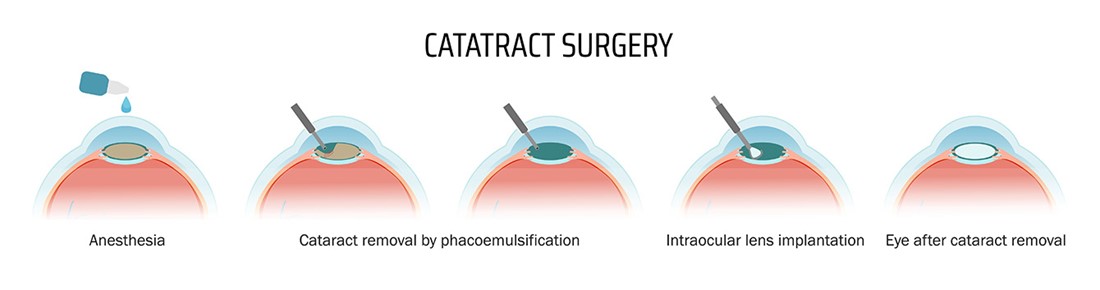 Cataract Surgery Diagram
Cataract Surgery Diagram
Top Intraoperative Complications of Cataract Surgery
- Posterior Capsule Rupture: One of the most common complications during cataract surgery, this occurs when the thin capsular membrane behind the lens tears, possibly causing lens fragments to enter the vitreous cavity. This raises the risk of retinal detachment and may necessitate further surgical intervention.
There is nationally published data on rates of posterior capsule rupture. Whilst the national standard is 1.95%, Moorfields Eye hospital reported a rate of 0.88% over 2023/24. In his most recent review of complications, Mr Modi has a 0% rate of posterior capsular rupture in August 2024 to August 2025 year.
- Vitreous Loss: If the posterior capsule ruptures, the gel-like vitreous can move forward, leading to inflammation, increased eye pressure, and heightened infection risk. Skilled handling by the surgeon is crucial to minimise further complications.
- Suprachoroidal Haemorrhage: Rare but serious, this bleeding between the choroid and sclera, two layers at the back of the eye, can cause sudden eye pain and vision loss. Risk factors include older age, glaucoma, and high blood pressure. Immediate medical attention is vital and again, if recognised early during surgery, steps can be taken to minimise the risk to vision.
Mr Modi has a 0% rate of complication for the above three intraoperative complications from August 2024 to August 2025 year.
Early Postoperative Complications After Cataract Surgery
- Endophthalmitis: A rare but potentially blinding infection, endophthalmitis presents with worsening pain, redness, and reduced vision after surgery. Urgent treatment with antibiotics and sometimes surgery is required to save vision.
- Cystoid Macular Oedema (CMO): CMO refers to fluid build-up in the retina’s central area, causing blurred or wavy vision. It is more common in patients with diabetes or complex surgeries and is typically managed with anti-inflammatory drops.
- Persistent Corneal Oedema: Swelling of the cornea can result from surgical trauma. Symptoms include hazy vision and discomfort. While most cases resolve, persistent corneal oedema may require further treatments such as corneal transplantation.
Mr Modi has a 0% rate of complication for the above three early postoperative complications from August 2024 to August 2025 year.
Late Postoperative Complications of Cataract Surgery
- Retinal Detachment: Though uncommon, retinal detachment is a serious risk, especially in patients with high myopia or posterior capsule rupture. Symptoms include flashes, floaters, or a shadow over vision, requiring prompt surgical repair.
- Intraocular Lens (IOL) Dislocation: The artificial lens can sometimes move out of place due to weak support or trauma, leading to vision problems. In such cases, surgical correction may be necessary.
Mr Modi has a 0% rate of complication for both of the above late postoperative complications from August 2024 to August 2025 year.
How to Minimise Cataract Surgery Risks
- Choose an experienced eye surgeon with an excellent track record to ensure the highest standard of care.
- Preoperative assessment and planning and assessment is key and ideally you would see the same person through the whole journey, from preassessment, through surgery and on for follow up. This allows the patient and eye to be optimised for surgery and keeps risks and therefore complications to a minimum.
- Attend all preoperative assessments to identify and manage underlying health risks before surgery. One of the main risks of having infection is blepharitis. Treating this thoroughly prior to surgery is important in reducing the risk of infection.
- Follow postoperative instructions carefully and attend all follow-up appointments for early detection of complications.
- Report any symptoms such as pain, redness, vision changes, flashes, or floaters immediately to your eye care provider.
Conclusion
Cataract surgery offers transformative results for patients with vision impairment. While serious complications are rare, understanding the main risks—posterior capsule rupture, vitreous loss, endophthalmitis, cystoid macular oedema, corneal oedema, retinal detachment, and IOL dislocation—empowers you to make informed decisions.
