Minimally Invasige Glaucoma Surgery
Minimally Invasive Glaucoma Surgery (MIGS) refers to a range of procedures rather than a single operation. They all aim to lower the eye pressure (Intraocular pressure or IOP) snd they do this by reducing the resistance to fluid drainage out of the eye.
Lowering the pressure in the eye is the mainstay of treatment for glaucoma, and this in turn reduces the progressive damage to the optic nerve and therefore reduces the loss of vision.
They are all minimally invasive because they use small incisions and therefore have a lower risk compared to larger surgeries such as trabeculectomy or aqueous shunt.
The following procedures come under the umbrella of MIGS procedures:
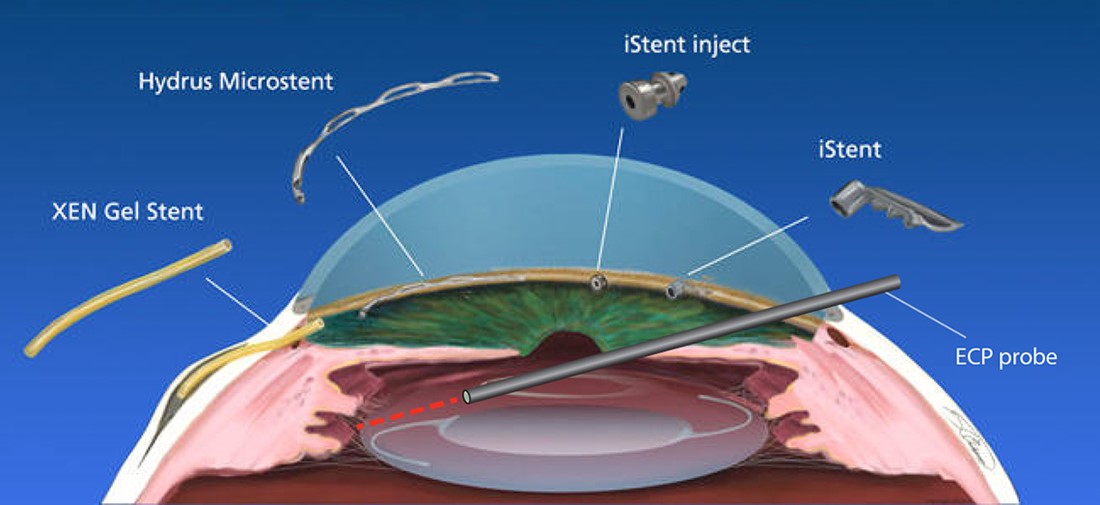
iStent
This is a tiny (1mm) titanium tube that is placed into the trabecular meshwork of the eye and therefore bypasses one of the areas of resistance to the drainage of fluid out of the eye. They stay in place in the trabecular meshwork and are usually placed as a pair.
These stents have been around longer than most of the others and over 1 million have been used worldwide. They have a good safety profile, are NICE (National Institute of Health and Care Excellence) approved and have little side effect.
These can be inserted at the same time as cataract surgery though the same 2.2 mm incision and may help further lower eye pressure.
Hydrus
This device is similar to the iStent in that it bypasses resistance at the level of the trabecular meshwork and is placed in the canal of Schlemm with an opening into the anterior chamber of the eye.
It is larger than an iStent and is about the size of an eyelash. This sits in the canal of Schlemm and holds the channel open. It is made of a nickel-aluminium alloy and is placed in the eye though an additional small incision.
Again, these have a good safety profile and are NICE (National Institute of Health and Care Excellence) approved.
Ab-interno Canaloplasty (with iTrack or OMNI)
The canaloplasty clears the canal of Schlemm, which is part of the drainage system of the eye. This is done from inside the eye rather than from the side, using a gonioscope (a special lens used to look at the drainage system of the eye) hence ‘ab-interno’ if you know your Latin.
Both iTrack and OMNI use a small catheter (tube), which is placed into the canal of Schlemm and a gel is injected through the catheter, which opens up the drainage channel and breaks/stretches open any narrowings along the channel. The flow of fluid out of the eye is therefore enhanced.
This procedure can be performed at the same time as cataract surgery though the same 2.2incision and may help further lower eye pressure.
The benefit of this over the iStent or the Hydrus is that no metal devices are left behind inside the eye. It also means that a stent can be subsequently be placed
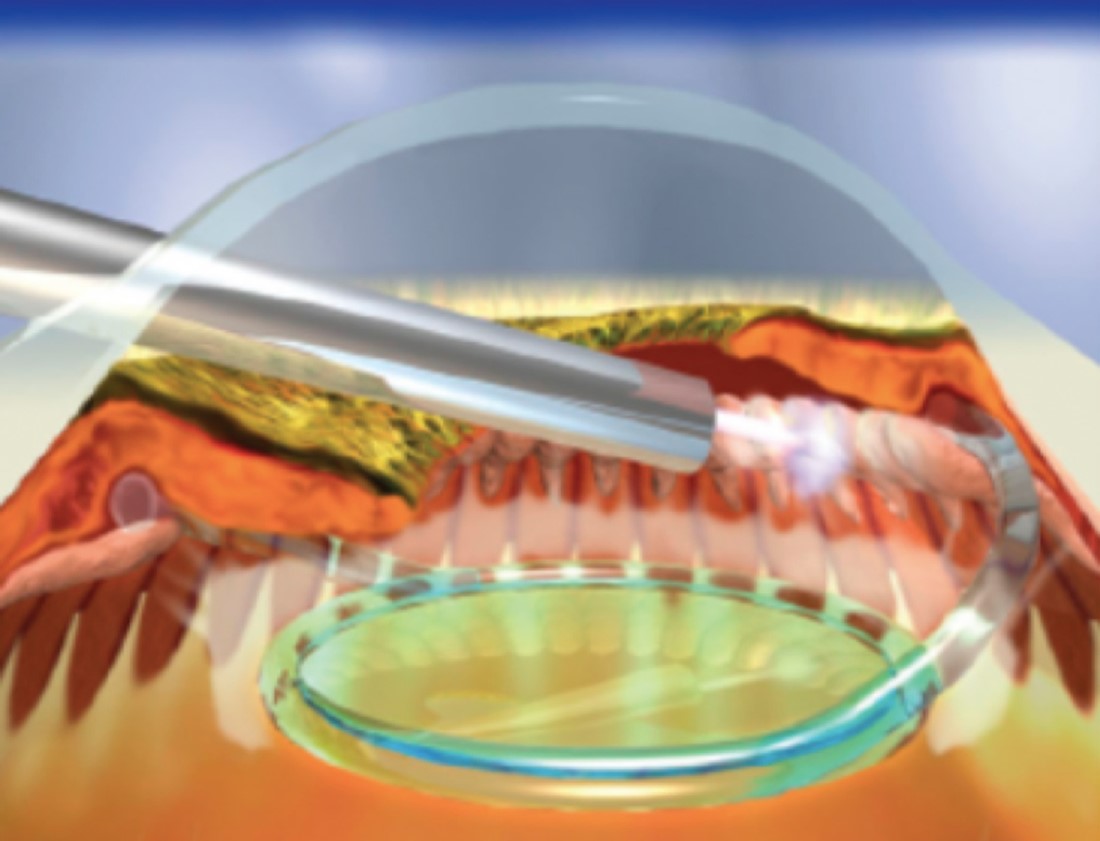
Endoscopic Cyclophotocoagulation (ECP)
ECP uses a laser probe to ‘coagulate’ or burn parts of the ciliary body. This is a part of the ey which produces fluid, this by lasering it the fluid production decreases and the pressure reduces. This again can be performed combined with cataract surgery through a small incision.
The main advantage over the other procedures listed is that this can be performed in patients with narrow or closed angle forms of glaucoma. The other stents are only possible to use in an open angle glaucoma. This is because the ciliary body is behind the lens so we are not relying on an open angle.
The disadvantage is that cataract surgery or lens extraction needs to be performed because the get to the ciliary body, one needs to go under the lens. Many of the other procedures can be performed independently of cataract surgery if required.
ECP also causes more inflammation than the other procedures so an extended course of postoperative steroid drops (6 weeks rather than 4 weeks) is usually given.
Xen Gel Implant
The Xen gel implant (pronounced Zen) is a tiny tube that is placed inside the eye and drains fluid out into the conjunctiva or sub-tenon’s space. It forms a small area which looks like a blister, known as a ‘bleb.’ It is made of denatured porcine gelatin (derived from pigs) and is used in conjunction with an anti-scarring drug (Mitomycin C).
Preserflo Microshunt
This is a small tube, much like the Xen gel stent, and is inserted to create a new passageway from inside to the soutside sub conjunctival or sub tenon’s space. It again forms a bleb, which sits under the upper eyelid. This improves drainage of fluid out of the eye and reduces they IOP. It is made of plastic and is used in combination with an anti-scarring drug (Mitomycin C).
MIGS FAQs
Who is suitable for MIGS?
There is a MIGS procedure that is suitable for anyone who is able to have cataract surgery and often the MIGS procedure is performed through the same incision. This gives the patient the added benefit of having better IOP control as well as better vision from their cataract surgery.
Cataract surgery itself lowere eye pressure by 1-2 mmHg but this effect is often short -lived and adding a MIGS procedure helps increase and prolong this effect.
What are the alternatives?
The alternatives include Selective Laser Trabeculoplasty (SLT) and conventional surgery such as trabeculectomy. These will be discussed with you in clinic if deemed appropriate.
Will I need general anaesthetic?
No – you can have MIGS under local anaesthetic as with cataract surgery. Although if you prefer, a general anaesthetic can also be used. The procedures are usually short and only add 10-15 minutes to a cataract operation.
What is the follow-up?
There is usually a follow up at around day 1-3, to ensure the pressure does not increase, which It can do transiently after any of these procedures. Subsequently there are appointments at around 1 week and then 1 month.
Will my vision improve?
Any loss of field of vision from glaucoma is irreversible. This is why it is important to diagnose and treat this early and effectively.
If combined with cataract surgery, the vision will improve as a result of the cataract removal as well as correction of any myopia/hypermetropia or astigmatism.
Can I stop my eye drops after the operation?
Postoperatively, antibiotics and steroids are prescribed for 4-8 weeks. After that, in some cases the eye drops may be stopped but ongoing follow up will always be required and any reduction in eye drops may not be permanent. The effect of a MIGS procedure is on average, similar to removing one eye drop. So, if for example, prior to surgery several drops were being used, it may mean the number of drops can be reduced but not stopped completely. This does mean that if a step-up in treatment is needed in years to come, a further drop can potentially be added rather than needing a further surgery.
Importantly, the normal glaucoma drops are continued after surgery and in the operated eye, a fresh bottle is usually advised for 2 weeks postoperatively to reduce the risk of cross-infection. After 2 weeks, the eye is relatively well healed and the same bottle can be used across both eyes.